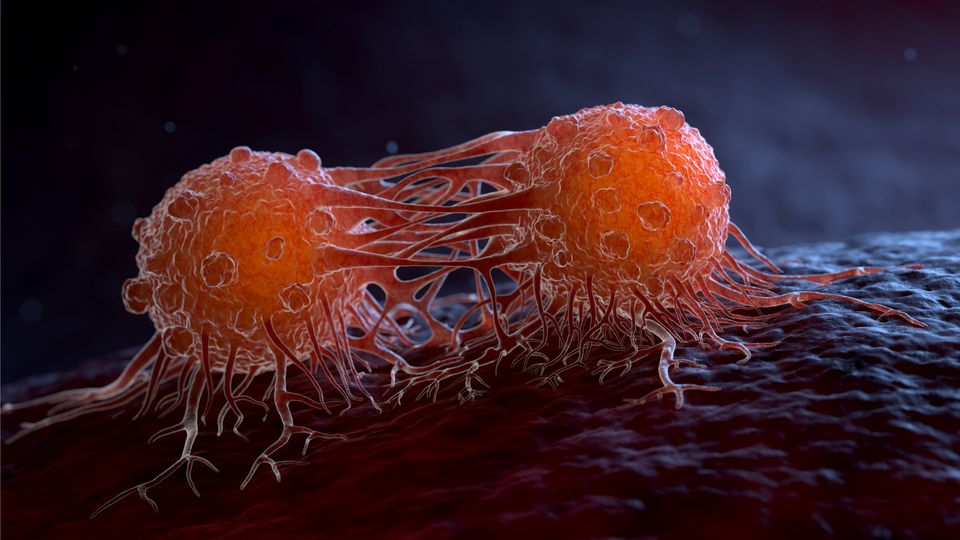
Cancer (medical term: malignant neoplasm) is a class of diseases in which a group of cells display uncontrolled growth (division beyond the normal limits), invasion (intrusion on and destruction of adjacent tissues), and sometimes metastasis (spread to other locations in the body via lymph or blood). These three malignant properties of cancers differentiate them from benign tumors, which are self-limited, and do not invade or metastasize. Most cancers form a tumor but some, like leukemia, do not. The branch of medicine concerned with the study, diagnosis, treatment, and prevention of cancer is oncology.
Cancer affects people at all ages with the risk for most types increasing with age. Cancer caused about 13% of all human deaths in 2007 (7.6 million).
Cancers are caused by abnormalities in the genetic material of the transformed cells. These abnormalities may be due to the effects of carcinogens, such as tobacco smoke, radiation, chemicals, or infectious agents. Other cancer-promoting genetic abnormalities may randomly occur through errors in DNA replication, or are inherited, and thus present in all cells from birth. The heritability of cancers is usually affected by complex interactions between carcinogens and the host’s genome.
Genetic abnormalities found in cancer typically affect two general classes of genes. Cancer-promoting oncogenes are typically activated in cancer cells, giving those cells new properties, such as hyperactive growth and division, protection against programmed cell death, loss of respect for normal tissue boundaries, and the ability to become established in diverse tissue environments. Tumor suppressor genes are then inactivated in cancer cells, resulting in the loss of normal functions in those cells, such as accurate DNA replication, control over the cell cycle, orientation and adhesion within tissues, and interaction with protective cells of the immune system.
Definitive diagnosis requires the histologic examination of a biopsy specimen, although the initial indication of malignancy can be symptomatic or radiographic imaging abnormalities. Most cancers can be treated and some forced into remission, depending on the specific type, location, and stage. Once diagnosed, cancer is usually treated with a combination of surgery, chemotherapy and radiotherapy. As research develops, treatments are becoming more specific for different varieties of cancer. There has been significant progress in the development of targeted therapy drugs that act specifically on detectable molecular abnormalities in certain tumors, and which minimize damage to normal cells. The prognosis of cancer patients is most influenced by the type of cancer, as well as the stage, or extent of the disease. In addition, histologic grading and the presence of specific molecular markers can also be useful in establishing prognosis, as well as in determining individual treatments.
What are the Causes and Risk Factors for Cancer?
Cells are the building blocks of living things. Cancer grows out of normal cells in the body. Normal cells multiply when the body needs them, and die when the body doesn’t need them. Cancer appears to occur when the growth of cells in the body is out of control and cells divide too quickly. It can also occur when cells “forget” how to die.
Cancer is a diverse class of diseases which differ widely in their causes and biology. Any organism, even plants, can acquire cancer. Nearly all known cancers arise gradually, as errors build up in the cancer cell and its progeny.
Anything which replicates (living cells) will probabilistically suffer from errors (mutations). Unless error correction and prevention is properly carried out, the errors will survive, and might be passed along to daughter cells. Normally, the body safeguards against cancer via numerous methods, such as: apoptosis, helper molecules (some DNA polymerases), possibly senescence, etc. However these error-correction methods often fail in small ways, especially in environments that make errors more likely to arise and propagate. For example, such environments can include the presence of disruptive substances called carcinogens, or periodic injury (physical, heat, etc.), or environments that cells did not evolve to withstand, such as hypoxia (see subsections). Cancer is thus a progressive disease, and these progressive errors slowly accumulate until a cell begins to act contrary to its function in the organism.
The errors which cause cancer are often self-amplifying, eventually compounding at an exponential rate. For example:
- A mutation in the error-correcting machinery of a cell might cause that cell and its children to accumulate errors more rapidly
- A mutation in signaling (endocrine) machinery of the cell can send error-causing signals to nearby cells
- A mutation might cause cells to become neoplastic, causing them to migrate and disrupt more healthy cells
- A mutation may cause the cell to become immortal, causing them to disrupt healthy cells forever
Thus cancer often explodes in something akin to a chain reaction caused by a few errors, which compound into more severe errors. Errors which produce more errors are effectively the root cause of cancer, and also the reason that cancer is so hard to treat: even if there were 10,000,000,000 cancerous cells and one killed all but 10 of those cells, those cells (and other error-prone precancerous cells) could still self-replicate or send error-causing signals to other cells, starting the process over again. This rebellion-like scenario is an undesirable survival of the fittest, where the driving forces of evolution work against the body’s design and enforcement of order. In fact, once cancer has begun to develop, this same force continues to drive the progression of cancer towards more invasive stages, and is called clonal evolution.
Research about cancer causes often falls into the following categories:
- Agents (e.g. viruses) and events (e.g. mutations) which cause or facilitate genetic changes in cells destined to become cancer.
- The precise nature of the genetic damage, and the genes which are affected by it.
- The consequences of those genetic changes on the biology of the cell, both in generating the defining properties of a cancer cell, and in facilitating additional genetic events which lead to further progression of the cancer.
Chemicals
Cancer pathogenesis is traceable back to DNA mutations that impact cell growth and metastasis. Substances that cause DNA mutations are known as mutagens, and mutagens that cause cancers are known as carcinogens. Particular substances have been linked to specific types of cancer. Tobacco smoking is associated with many forms of cancer, and causes 90% of lung cancer. Prolonged exposure to asbestos fibers is associated with mesothelioma.
Many mutagens are also carcinogens, but some carcinogens are not mutagens. Alcohol is an example of a chemical carcinogen that is not a mutagen. Such chemicals may promote cancers through stimulating the rate of cell division. Faster rates of replication leaves less time for repair enzymes to repair damaged DNA during DNA replication, increasing the likelihood of a mutation.
Decades of research has demonstrated the link between tobacco use and cancer in the lung, larynx, head, neck, stomach, bladder, kidney, oesophagus and pancreas. Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons. Tobacco is responsible for about one in three of all cancer deaths in the developed world, and about one in five worldwide. Indeed, lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently, decreases in smoking followed by decreases in lung cancer death rates in men. However, the numbers of smokers worldwide is still rising, leading to what some organizations have described as the tobacco epidemic.
Ionizing radiation
Sources of ionizing radiation, such as radon gas, can cause cancer. Prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies. It is estimated that 2% of future cancers will be due to current CT scans.
Non-ionizing radio frequency radiation from mobile phones and other similar RF sources has also been proposed as a cause of cancer, but there is currently little established evidence of such a link.
Infection
Some cancers can be caused by infection. This is especially true in animals such as birds, but also in humans, with viruses responsible for up to 20% of human cancers worldwide. These include human papillomavirus (cervical carcinoma), human polyomaviruses (mesothelioma, brain tumors), Epstein-Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma), Kaposi’s sarcoma herpesvirus (Kaposi’s Sarcoma and primary effusion lymphomas), hepatitis B and hepatitis C viruses (hepatocellular carcinoma), Human T-cell leukemia virus-1 (T-cell leukemias), and Helicobacter pylori (gastric carcinoma).
Experimental and epidemiological data imply a causative role for viruses and they appear to be the second most important risk factor for cancer development in humans, exceeded only by tobacco usage. The mode of virally induced tumors can be divided into two, acutely transforming or slowly transforming. In acutely transforming viruses, the virus carries an overactive oncogene called viral-oncogene (v-onc), and the infected cell is transformed as soon as v-onc is expressed. In contrast, in slowly transforming viruses, the virus genome is inserts near a proto-oncogene in the host genome. The viral promoter or other transcription regulation elements then cause overexpression of that proto-oncogene. This induces uncontrolled cell division. Because the site of insertion is not specific to proto-oncogenes and the chance of insertion near any proto-oncogene is low, slowly transforming viruses will cause tumors much longer after infection than the acutely transforming viruses.
Hepatitis viruses, including hepatitis B and hepatitis C, can induce a chronic viral infection that leads to liver cancer in 0.47% of hepatitis B patients per year (especially in Asia, less so in North America), and in 1.4% of hepatitis C carriers per year. Liver cirrhosis, whether from chronic viral hepatitis infection or alcoholism, is associated with the development of liver cancer, and the combination of cirrhosis and viral hepatitis presents the highest risk of liver cancer development. Worldwide, liver cancer is one of the most common, and most deadly, cancers due to a huge burden of viral hepatitis transmission and disease.
Advances in cancer research have made a vaccine designed to prevent cancer available. In 2006, the U.S. Food and Drug Administration approved a human papilloma virus vaccine, called Gardasil. The vaccine protects against four HPV types, which together cause 70% of cervical cancers and 90% of genital warts. In March 2007, the US Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) officially recommended that females aged 11–12 receive the vaccine, and indicated that females as young as age 9 and as old as age 26 are also candidates for immunization.
In addition to viruses, researchers have noted a connection between bacteria and certain cancers. The most prominent example is the link between chronic infection of the wall of the stomach with Helicobacter pylori and gastric cancer. Although only a minority of those infected with Helicobacter go on to develop cancer, since this pathogen is quite common it is probably responsible for most of these cancers.
Hormonal imbalances
Some hormones can act in a similar manner to non-mutagenic carcinogens in that they may stimulate excessive cell growth.
Immune system dysfunction
HIV is associated with a number of malignancies, including Kaposi’s sarcoma, non-Hodgkin’s lymphoma, and HPV-associated malignancies such as anal cancer and cervical cancer. AIDS-defining illnesses have long included these diagnoses. The increased incidence of malignancies in HIV patients points to the breakdown of immune surveillance as a possible etiology of cancer. Certain other immune deficiency states (e.g. common variable immunodeficiency and IgA deficiency) are also associated with increased risk of malignancy.
Heredity
Most forms of cancer are sporadic, meaning that there is no inherited cause of the cancer. There are, however, a number of recognised syndromes where there is an inherited predisposition to cancer, often due to a defect in a gene that protects against tumor formation. Famous examples are:
- certain inherited mutations in the genes BRCA1 and BRCA2 are associated with an elevated risk of breast cancer and ovarian cancer
- tumors of various endocrine organs in multiple endocrine neoplasia (MEN types 1, 2a, 2b)
- Li-Fraumeni syndrome (various tumors such as osteosarcoma, breast cancer, soft tissue sarcoma, brain tumors) due to mutations of p53
- Turcot syndrome (brain tumors and colonic polyposis)
- Familial adenomatous polyposis an inherited mutation of the APC gene that leads to early onset of colon carcinoma.
- Hereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch syndrome) can include familial cases of colon cancer, uterine cancer, gastric cancer, and ovarian cancer, without a preponderance of colon polyps.
- Retinoblastoma, when occurring in young children, is due to a hereditary mutation in the retinoblastoma gene.
- Down syndrome patients, who have an extra chromosome 21, are known to develop malignancies such as leukemia and testicular cancer, though the reasons for this difference are not well understood.
Other causes
Excepting the rare transmissions that occur with pregnancies and only a marginal few organ donors, cancer is generally not a transmissible disease. The main reason for this is tissue graft rejection caused by MHC incompatibility. In humans and other vertebrates, the immune system uses MHC antigens to differentiate between “self” and “non-self” cells because these antigens are different from person to person. When non-self antigens are encountered, the immune system reacts against the appropriate cell. Such reactions may protect against tumour cell engraftment by eliminating implanted cells. In the United States, approximately 3,500 pregnant women have a malignancy annually, and transplacental transmission of acute leukaemia, lymphoma, melanoma and carcinoma from mother to fetus has been observed. The development of donor-derived tumors from organ transplants is exceedingly rare. The main cause of organ transplant associated tumors seems to be malignant melanoma, that was undetected at the time of organ harvest. though other cases exist In fact, cancer from one organism will usually grow in another organism of that species, as long as they share the same histocompatibility genes, proven using mice; however this would never happen in a real-world setting except as described above.
In non-humans, a few types of transmissible cancer have been described, wherein the cancer spreads between animals by transmission of the tumor cells themselves. This phenomenon is seen in dogs with Sticker’s sarcoma, also known as canine transmissible venereal tumor, as well as Devil facial tumour disease in Tasmanian devils.
What are the most common Types of Cancer?
Skin cancer is the most commonly diagnosed cancer among men and women. Over one million cases are diagnosed each year, with more young people having skin cancer than ever before. The most common types of cancer in the United States based on frequency of diagnosis are:
- bladder cancer
- breast cancer
- colon cancer
- endometrial cancer
- kidney cancer (renal cell)
- leukemia
- lung cancer
- melanoma
- non-Hodgkin lymphoma
- pancreatic cancer
- prostate cancer
- thyroid cancer
Types of Cancer Classified by Body System
Cancer has the potential to affect every organ in the body. The cells within malignant tumors have the ability to invade neighboring tissues and organs, thus spreading the disease. It is also possible for cancerous cells to break free from the tumor and enter the bloodstream, in turn spreading the disease to other organs. This process of spreading is called metastasis.
When cancer has metastasized and has affected other areas of the body, the disease is still referred to the organ of origination. For instance, if cervical cancer spreads to the lungs, it is still called cervical cancer, not lung cancer.
Blood Cancer: The cells in the bone marrow that give rise to red blood cells, white blood cells, and platelets can sometimes become cancerous. These cancers are leukemia or lymphoma.
- Leukemia
- Lymphoma
- Multiple Myeloma
- Waldenstrom’s Macroglobulinemia
Bone Cancer: Bone cancer is a relatively rare type of cancer that can affect both children and adults, but primarily affects children and teens. There are several types of bone cancer, but the most common types are:
- Ewing’s Sarcoma
- Osteosarcoma
Brain Cancer: Brain tumors can be malignant (cancerous) or benign (non-cancerous). They affect both children and adults. Malignant brain tumors don’t often spread beyond the brain. However, other types of cancer have the ability to spread to the brain. Types of brain cancer include:
- Adult Brain Tumor
- Brain Stem Glioma, Childhood
- Cerebellar Astrocytoma, Childhood
- Cerebral Astrocytoma/Malignant Glioma, Childhood
- Ependymoma, Childhood
- Medulloblastoma, Childhood
- Supratentorial Primitive Neuroectodermal Tumors and Pineoblastoma, Childhood
- Visual Pathway and Hypothalamic Glioma, Childhood
Breast Cancer: Breast cancer is a common type of cancer that affects women and much less commonly, men. More than 200,000 women are diagnosed with breast cancer in the United States each year. Types of breast cancer include, but are not limited to:
- ductal carcinoma in situ
- lobular carcinoma in situ
- inflammatory breast cancer
- Paget’s disease of the nipple
- Invasive types of breast cancer
Digestive/Gastrointestinal Cancers This is a broad category of cancer that affects everything from the esophagus to the anus. Each type is specific and has its own symptoms, causes, and treatments.
- Anal Cancer
- Bile Duct Cancer, Extrahepatic
- Carcinoid Tumor, Gastrointestinal
- Colon Cancer
- Esophageal Cancer
- Gallbladder Cancer
- Liver Cancer, Adult Primary
- Liver Cancer, Childhood
- Pancreatic Cancer
- Rectal Cancer
- Small Intestine Cancer
- Stomach (Gastric) Cancer
Endocrine Cancers: The endocrine system is an instrumental part of the body that is responsible for glandular and hormonal activity. Thyroid cancer is the most common of the endocrine cancer types and generally, the least fatal.
- Adrenocortical Carcinoma
- Carcinoid Tumor, Gastrointestinal
- Islet Cell Carcinoma (Endocrine Pancreas)
- Parathyroid Cancer
- Pheochromocytoma
- Pituitary Tumor
- Thyroid Cancer
Eye Cancer: Like other organs in the human body, the eyes are vulnerable to cancer as well. Eye cancer can affect both children and adults.
- Melanoma, Intraocular
- Retinoblastoma
Genitourinary Cancers: These types of cancer affect the male genitalia and urinary tract.
- Bladder Cancer
- Kidney (Renal Cell) Cancer
- Penile Cancer
- Prostate Cancer
- Renal Pelvis and Ureter Cancer, Transitional Cell
- Testicular Cancer
- Urethral Cancer
- Wilms’ Tumor and Other Childhood Kidney Tumors
Gynecologic Cancers: This group of cancer types affect the organs of the female reproductive system. Specialized oncologists called gynecologic oncologists are recommended for treating gynecologic cancer.
- Cervical Cancer
- Endometrial Cancer
- Gestational Trophoblastic Tumor
- Ovarian Cancer
- Uterine Sarcoma
- Vaginal Cancer
- Vulvar Cancer
Head and Neck Cancer: Most head and neck cancers affect moist mucosal surfaces of the head and neck, like the mouth, throat, and nose. Causes of head and neck cancer vary, but cigarette smoking plays a role. Current research suggests a strong HPV link in the development of some head and neck cancer.
- Hypopharyngeal Cancer
- Laryngeal Cancer
- Lip and Oral Cancer
- Metastatic Squamous Neck Cancer
- Nasopharyngeal Cancer
- Oropharyngeal Cancer
- Paranasal Sinus and Nasal Cavity Cancer
- Parathyroid Cancer
- Salivary Gland Cancer
Respiratory Cancers: Cigarette smoking is the primary cause for cancer affecting the respiratory system. Exposure to asbestos is also a factor.
- Lung Cancer, Non-Small Cell
- Lung Cancer, Small Cell
- Malignant Mesothelioma
- Thymoma and Thymic Carcinoma
Skin Cancers:
Non-melanoma skin cancer is the most common type of cancer among men and women. Exposure to the UV rays of the sun is the primary cause for non-melanoma skin cancer and also melanoma.
- Cutaneous T-Cell Lymphoma
- Kaposi’s Sarcoma
- Melanoma
- Merkel Cell Carcinoma
- Non-Melanoma Skin Cancer
What are the symptoms of Cancer?
A broad spectrum of non-specific cancer symptoms may include:
- Persistent Fatigue: Fatigue is one of the most commonly experienced cancer symptoms. It is usually more common when the cancer is advanced, but still occurs in the early stages of some cancers. Anemia is commonly the culprit — a condition that is associated with many types of cancer, especially types affecting the bowel. Fatigue is a symptom of both malignant and non-malignant conditions and should be evaluated by a physician.
- Unintentional Weight Loss: While it may be a welcome surprise to lose weight without trying, it can be a red flag for many illnesses, including cancer. Losing 10 pounds or more unintentionally definitely warrants a visit to the doctor. This type of weight loss can occur with or without loss of appetite. Remember, weight loss can be a symptom of cancer, but is also a symptom of many other illnesses, too.
- Pain Typically, pain is not an early symptom of cancer, except in some cancer types like those that spread to the bone. Pain generally occurs when cancer spreads and begins to affect other organs and nerves.
Lower pack pain is cancer symptom that is associated with ovarian cancer and colon cancer. Shoulder pain can also be a symptom of lung cancer. Pain in the form of headaches can be associated with brain tumors (malignant and benign).
Stomach pains can be related to types of cancer, like stomach cancer, pancreatic cancer, and many others. Stomach pain can be a very vague symptom because so many illnesses can cause stomach pain. - Fever: A fever is a very non-specific symptom of many mild to severe conditions, including cancer. In relation to cancer, a fever that is persistent or one that comes and goes frequently can signal stress on the immune system. Fevers are commonly associated with types of cancer that affects the blood, like leukemia and lymphoma, but are also common in people whose cancer has spread.
- Bowel Changes: If you experience constipation, diarrhea, blood in the stools, gas, thinner stools, or just a general overall change in bowel habits, see your doctor. These symptoms are most commonly associated with colon cancer, but are also related to other cancer types.
- Chronic Cough: A persistent, new cough or a cough that won’t go away or becomes worse needs to be evaluated by a doctor. Blood and/or mucus may accompany the cough and can be caused many conditions. In relation to cancer, a chronic cough with blood or mucus can be symptom of lung cancer.
Keep in mind that these are very general, vague symptoms of cancer. If you have one or two of these symptoms, it is not a red flag for cancer but more an indication to your doctor to run certain medical tests. The symptoms listed above are experienced by most people with cancer at various stages of their disease, but are also linked to many other non-cancerous conditions. For more specific cancer symptoms, see below for symptom information about several types of cancer.
Methods of Treatment for Cancer
There are four standard methods of treatment for cancer: surgery, chemotherapy, radiation therapy, immunotherapy and biologic therapy. Clinical trials may be an option for some as cancer treatment who meet certain study criteria. Others may choose alternative cancer treatments, which are usually not FDA-approved and often given in locations outside of the U.S.
When initially diagnosed with cancer, a cancer specialist, an oncologist, will provide you with the cancer treatment options. He or she will recommend the best treatment plan based on your type of cancer, how far it has spread, and other important factors like your age and general health.
Ultimately, you are the one who makes your treatment decisions based on your doctor’s recommendations, possible second opinions, and other information gathered from qualified professionals.
Surgery: Surgery can be used to prevent, treat, stage (determine how advanced the cancer is), and diagnose cancer. In relation to cancer treatment, surgery is done to remove tumors or as much of the cancerous tissue as possible. It is often performed in conjunction with chemotherapy or radiation therapy.
For those whose cancer is not treatable, palliative surgery may be an option to relieve pain that may be caused by the cancer. Palliative surgery is not intended to treat or cure the cancer, or even to prolong life, but more to lessen discomfort.
Chemotherapy: Chemotherapy is a type of cancer treatment that uses of drugs to eliminate cancer cells. Unlike surgery, chemotherapy affects the entire body, not just a specific part. It works by targeting rapidly multiplying cancer cells. Unfortunately, other types of cells in our bodies also multiply at high rates, like hair follicle cells and the cells that line our stomachs. This is why chemo can cause side effects like hair loss and an upset stomach.
Chemotherapy is most commonly given by pill or intravenously (IV), but can be given in other ways. A single type of chemotherapy, or a combination of drugs, may be prescribed for a specific length of time. Like surgery, chemotherapy can be prescribed alone, in conjunction with radiation therapy or biologic therapy.
Radiation Therapy: Radiation therapy uses certain types of energy to shrink tumors or eliminate cancer cells. It works by damaging a cancer cell’s DNA, making it unable to multiply. Cancer cells are highly sensitive to radiation and typically die when treated. Nearby healthy cells can be damaged as well, but are resilient and are able to fully recover.
Radiation therapy may be given alone, along with chemotherapy, and/or with surgery. The decision to combine radiation therapy with other types of treatment depends on the stage of cancer and other factors.
Biologic or Targeted Therapy:
Biologic therapy is a term for drugs that target characteristics of cancerous tumors. Some types of targeted therapies work by blocking the biological processes of tumors that allow tumors to thrive and grow. Other types of therapies cut off the blood supply to the tumor, causing it to basically starve and die because of a lack of blood.
Targeted therapy is used in select types of cancer and is not available for everyone. It is given in conjunction with other cancer treatments.
Clinical Trials: Research studies of the latest drugs and therapies against many types of cancer are continuously being conducted. This type of research requires human volunteers to test the safety and effectiveness of new therapies. Volunteers must meet the criteria of each study to participate.
Drugs rating:
| Title | Votes | Rating | ||
| 1 | Cenestin (Conjugated Estrogens) | 8 |
|
(10.0/10) |
| 2 | Leukeran (Chlorambucil) | 2 |
|
(10.0/10) |
| 3 | Menest (Esterified Estrogens) | 1 |
|
(10.0/10) |
| 4 | Carac Cream (Fluorouracil) | 1 |
|
(10.0/10) |
| 5 | Delestrogen (Estradiol Valerate) | 6 |
|
(9.3/10) |
| 6 | Adriamycin (Doxorubicin) | 11 |
|
(8.9/10) |
| 7 | Eulexin (Flutamide) | 2 |
|
(8.5/10) |
| 8 | Velcade (Bortezomib) | 16 |
|
(8.4/10) |
| 9 | Estrace (Estradiol) | 16 |
|
(8.3/10) |
| 10 | Megace (Megestrol) | 3 |
|
(8.3/10) |
| 11 | Sutent (Sunitinib) | 29 |
|
(8.2/10) |
| 12 | Enjuvia (Conjugated Estrogens) | 20 |
|
(8.2/10) |
| 13 | Xeloda (Capecitabine) | 25 |
|
(8.1/10) |
| 14 | Premarin (Conjugated Estrogens) | 57 |
|
(8.0/10) |
| 15 | Tarceva (Erlotinib) | 40 |
|
(8.0/10) |
| 16 | Nexavar (Sorafenib) | 11 |
|
(8.0/10) |
| 17 | Nolvadex (Tamoxifen) | 3 |
|
(8.0/10) |
| 18 | Arimidex (Anastrozole) | 145 |
|
(7.8/10) |
| 19 | Herceptin (Trastuzumab) | 36 |
|
(7.7/10) |
| 20 | Casodex (Bicalutamide) | 26 |
|
(7.7/10) |
| 21 | Faslodex (Fulvestrant) | 25 |
|
(7.7/10) |
| 22 | Firmagon (Degarelix) | 2 |
|
(7.5/10) |
| 23 | Soltamox (Tamoxifen) | 2 |
|
(7.5/10) |
| 24 | Efudex Cream (Fluorouracil) | 13 |
|
(7.4/10) |
| 25 | Aromasin (Exemestane) | 78 |
|
(7.2/10) |
| 26 | Torisel (Temsirolimus) | 13 |
|
(7.1/10) |
| 27 | Cytoxan (Cyclophosphamide) | 42 |
|
(7.0/10) |
| 28 | Doxil (Doxorubicin Liposomal) | 9 |
|
(7.0/10) |
| 29 | Provera (Medroxyprogesterone) | 122 |
|
(6.8/10) |
| 30 | Avastin (Bevacizumab) | 13 |
|
(6.8/10) |
| 31 | Femara (Letrozole) | 75 |
|
(6.7/10) |
| 32 | Lupron (Leuprolide) | 3 |
|
(6.7/10) |
| 33 | Methotrexate | 231 |
|
(6.5/10) |
| 34 | Novantrone (Mitoxantrone) | 55 |
|
(6.5/10) |
| 35 | Zoladex (Goserelin) | 47 |
|
(6.2/10) |
| 36 | Lupron Depot (Leuprolide) | 10 |
|
(6.2/10) |
| 37 | Taxol (Paclitaxel) | 13 |
|
(6.0/10) |
| 38 | Tamoxifen | 2 |
|
(6.0/10) |
| 39 | Fludara (Fludarabine) | 1 |
|
(6.0/10) |
| 40 | Erbitux (Cetuximab) | 10 |
|
(5.8/10) |
| 41 | Depo-Provera (Medroxyprogesterone) | 35 |
|
(5.7/10) |
| 42 | Camptosar (Irinotecan) | 1 |
|
(5.0/10) |
| 43 | Taxotere (Docetaxel) | 6 |
|
(4.3/10) |
| 44 | Fluoroplex Cream (Fluorouracil) | 1 |
|
(1.0/10) |
| 45 | Tace (Chlorotrianisene) | 0 |
|
(0/10) |
| 46 | Plenaxis (Abarelix) | 0 |
|
(0/10) |
| 47 | Trelstar (Triptorelin) | 0 |
|
(0/10) |
| 48 | Provenge (Sipuleucel-T) | 0 |
|
(0/10) |
| 49 | Trelstar LA (Triptorelin) | 0 |
|
(0/10) |
| 50 | Trelstar Depot (Triptorelin) | 0 |
|
(0/10) |
| 51 | Emcyt (Estramustine) | 0 |
|
(0/10) |
| 52 | Zanosar (Streptozocin) | 0 |
|
(0/10) |
| 53 | Pancreatin 4X (Pancreatin) | 0 |
|
(0/10) |
| 54 | Eligard (Leuprolide) | 0 |
|
(0/10) |
| 55 | Vantas (Histrelin Implant) | 0 |
|
(0/10) |
| 56 | Jevtana (Cabazitaxel) | 0 |
|
(0/10) |
| 57 | Gynodiol (Estradiol) | 0 |
|
(0/10) |
| 58 | Nilandron (Nilutamide) | 0 |
|
(0/10) |
| 59 | Mustargen (Mechlorethamine) | 0 |
|
(0/10) |
| 60 | Megace Suspension (Megestrol) | 0 |
|
(0/10) |
| 61 | Folotyn (Pralatrexate) | 0 |
|
(0/10) |
| 62 | Afinitor (Everolimus) | 0 |
|
(0/10) |
| 63 | PegIntron (Peginterferon Alfa-2b) | 0 |
|
(0/10) |
| 64 | Proleukin (Aldesleukin) | 0 |
|
(0/10) |
| 65 | Votrient (Pazopanib) | 0 |
|
(0/10) |
| 66 | Hexalen (Altretamine) | 0 |
|
(0/10) |
| 67 | Ontak (Denileukin Diftitox) | 0 |
|
(0/10) |
| 68 | Mithracin (Plicamycin) | 0 |
|
(0/10) |
| 69 | Blenoxane (Bleomycin) | 0 |
|
(0/10) |
| 70 | Oncovin (Vincristine) | 0 |
|
(0/10) |
| 71 | Vincasar PFS (Vincristine) | 0 |
|
(0/10) |
| 72 | Arranon (Nelarabine) | 0 |
|
(0/10) |
| 73 | Viadur Implant (Leuprolide) | 0 |
|
(0/10) |
| 74 | Tykerb (Lapatinib) | 0 |
|
(0/10) |
| 75 | Adrucil (Fluorouracil) | 0 |
|
(0/10) |
| 76 | Cytadren (Aminoglutethimide) | 0 |
|
(0/10) |
| 77 | Androxy (Fluoxymesterone) | 0 |
|
(0/10) |
| 78 | Fareston (Toremifene) | 0 |
|
(0/10) |
| 79 | Gemzar (Gemcitabine) | 0 |
|
(0/10) |
| 80 | Ixempra (Ixabepilone) | 0 |
|
(0/10) |
| 81 | Onxol (Paclitaxel) | 0 |
|
(0/10) |
| 82 | Neosar (Cyclophosphamide) | 0 |
|
(0/10) |
| 83 | Thiotepa | 0 |
|
(0/10) |
| 84 | Trexall (Methotrexate) | 0 |
|
(0/10) |
| 85 | Thioplex (Thiotepa) | 0 |
|
(0/10) |
| 86 | Velban (Vinblastine) | 0 |
|
(0/10) |
| 87 | Vinblastine | 0 |
|
(0/10) |
| 88 | Abraxane (Paclitaxel) | 0 |
|
(0/10) |
| 89 | Estratab (Esterified Estrogens) | 0 |
|
(0/10) |
| 90 | Etopophos (Etoposide) | 0 |
|
(0/10) |
| 91 | VePesid (Etoposide) | 0 |
|
(0/10) |
| 92 | Toposar (Etoposide) | 0 |
|
(0/10) |
| 93 | Alkeran (Melphalan) | 0 |
|
(0/10) |
| 94 | Cosmegen (Dactinomycin) | 0 |
|
(0/10) |
| 95 | Vectibix (Panitumumab) | 0 |
|
(0/10) |
| 96 | Eloxatin (Oxaliplatin) | 0 |
|
(0/10) |
| 97 | Mutamycin (Mitomycin) | 0 |
|
(0/10) |
| 98 | Platinol (Cisplatin) | 0 |
|
(0/10) |
| 99 | Paraplatin (Carboplatin) | 0 |
|
(0/10) |
| 100 | Hycamtin (Topotecan) | 0 |
|
(0/10) |
| 101 | Ifex (Ifosfamide) | 0 |
|
(0/10) |
| 102 | Ethyol (Amifostine) | 0 |
|
(0/10) |
Prevention
Cancer prevention is defined as active measures to decrease the incidence of cancer.Greater than 30% of cancer is preventable via avoiding risk factors including: tobacco, overweight or obesity, low fruit and vegetable intake, physical inactivity, alcohol, sexually transmitted infection, air pollution. This can be accomplished by avoiding carcinogens or altering their metabolism, pursuing a lifestyle or diet that modifies cancer-causing factors and/or medical intervention (chemoprevention, treatment of pre-malignant lesions). The epidemiological concept of “prevention” is usually defined as either primary prevention, for people who have not been diagnosed with a particular disease, or secondary prevention, aimed at reducing recurrence or complications of a previously diagnosed illness.
Modifiable factors
The vast majority of cancer risk factors are environmental or lifestyle-related, leading to the claim that cancer is a largely preventable disease. Examples of modifiable cancer risk factors include alcohol consumption (associated with increased risk of oral, esophageal, breast, and other cancers), smoking (80% of women with lung cancer have smoked in the past, and 90% of men), physical inactivity (associated with increased risk of colon, breast, and possibly other cancers), and being overweight / obese (associated with colon, breast, endometrial, and possibly other cancers). Based on epidemiologic evidence, it is now thought that avoiding excessive alcohol consumption may contribute to reductions in risk of certain cancers; however, compared with tobacco exposure, the magnitude of effect is modest or small and the strength of evidence is often weaker. Other lifestyle and environmental factors known to affect cancer risk (either beneficially or detrimentally) include certain sexually transmitted diseases (such as those conveyed by the human papillomavirus), the use of exogenous hormones, exposure to ionizing radiation and ultraviolet radiation from the sun or from tanning beds, and certain occupational and chemical exposures.
Every year, at least 200,000 people die worldwide from cancer related to their workplace. Millions of workers run the risk of developing cancers such as lung cancer and mesothelioma from inhaling asbestos fibers and tobacco smoke, or leukemia from exposure to benzene at their workplaces. Currently, most cancer deaths caused by occupational risk factors occur in the developed world. It is estimated that approximately 20,000 cancer deaths and 40,000 new cases of cancer each year in the U.S. are attributable to occupation.
Diet
The consensus on diet and cancer is that obesity increases the risk of developing cancer. Particular dietary practices often explain differences in cancer incidence in different countries (e.g. gastric cancer is more common in Japan, while colon cancer is more common in the United States. In this example the preceding consideration of Haplogroups are excluded). Studies have shown that immigrants develop the risk of their new country, often within one generation, suggesting a substantial link between diet and cancer. Whether reducing obesity in a population also reduces cancer incidence is unknown.
Despite frequent reports of particular substances (including foods) having a beneficial or detrimental effect on cancer risk, few of these have an established link to cancer. These reports are often based on studies in cultured cell media or animals. Public health recommendations cannot be made based on these studies until they have been validated in an observational (or occasionally a prospective interventional) trial in humans.
Proposed dietary interventions for primary cancer risk reduction generally gain support from epidemiological association studies. Examples of such studies include reports that reduced meat consumption is associated with decreased risk of colon cancer, and reports that consumption of coffee is associated with a reduced risk of liver cancer. Studies have linked consumption of grilled meat to an increased risk of stomach cancer, colon cancer, breast cancer, and pancreatic cancer, a phenomenon which could be due to the presence of carcinogens such as benzopyrene in foods cooked at high temperatures.
A 2005 secondary prevention study showed that consumption of a plant-based diet and lifestyle changes resulted in a reduction in cancer markers in a group of men with prostate cancer who were using no conventional treatments at the time. These results were amplified by a 2006 study. Over 2,400 women were studied, half randomly assigned to a normal diet, the other half assigned to a diet containing less than 20% calories from fat. The women on the low fat diet were found to have a markedly lower risk of breast cancer recurrence, in the interim report of December, 2006.
Recent studies have also demonstrated potential links between some forms of cancer and high consumption of refined sugars and other simple carbohydrates. Although the degree of correlation and the degree of causality is still debated, some organizations have in fact begun to recommend reducing intake of refined sugars and starches as part of their cancer prevention regimens.
In November 2007, the American Institute for Cancer Research (AICR), in conjunction with the World Cancer Research Fund (WCRF), published Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective, “the most current and comprehensive analysis of the literature on diet, physical activity and cancer”. The WCRF/AICR Expert Report lists 10 recommendations that people can follow to help reduce their risk of developing cancer, including the following dietary guidelines:
- reducing intake of foods and drinks that promote weight gain, namely energy-dense foods and sugary drinks,
- eating mostly foods of plant origin,
- limiting intake of red meat and avoiding processed meat,
- limiting consumption of alcoholic beverages, and
- reducing intake of salt and avoiding mouldy cereals (grains) or pulses (legumes).
Some mushrooms offer an anti-cancer effect, which is thought to be linked to their ability to up-regulate the immune system. Some mushrooms known for this effect include, Reishi, Agaricus blazei, Maitake, and Trametes versicolor. Research suggests the compounds in medicinal mushrooms most responsible for up-regulating the immune system and providing an anti-cancer effect, are a diverse collection of polysaccharide compounds, particularly beta-glucans. Beta-glucans are known as “biological response modifiers”, and their ability to activate the immune system is well documented. Specifically, beta-glucans stimulate the innate branch of the immune system. Research has shown beta-glucans have the ability to stimulate macrophage, NK cells, T cells, and immune system cytokines. The mechanisms in which beta-glucans stimulate the immune system is only partially understood. One mechanism in which beta-glucans are able to activate the immune system, is by interacting with the Macrophage-1 antigen (CD18) receptor on immune cells.
Vitamins
Vitamin supplementation has not been proven effective in the prevention of cancer. The components of food are also proving to be more numerous and varied than previously understood, so patients are increasingly advised to consume fruits and vegetables for maximal health benefits.
Vitamin D
Low levels of vitamin D is correlated with increased cancer risk. Whether this relationship is causal is yet to be determined.
Beta carotene
Beta-carotene supplementation has been found to increase slightly, but not significantly risks of lung cancer.
Folic acid
Folic acid supplementation has not been found effective in preventing colon cancer and may increase colon polyps.
Chemoprevention
The concept that medications could be used to prevent cancer is an attractive one, and many high-quality clinical trials support the use of such chemoprevention in defined circumstances.
Daily use of tamoxifen, a selective estrogen receptor modulator (SERM), typically for 5 years, has been demonstrated to reduce the risk of developing breast cancer in high-risk women by about 50%. A recent study reported that the selective estrogen receptor modulator raloxifene has similar benefits to tamoxifen in preventing breast cancer in high-risk women, with a more favorable side effect profile.
Raloxifene is a SERM like tamoxifen; it has been shown (in the STAR trial) to reduce the risk of breast cancer in high-risk women equally as well as tamoxifen. In this trial, which studied almost 20,000 women, raloxifene had fewer side effects than tamoxifen, though it did permit more DCIS to form.
Finasteride, a 5-alpha-reductase inhibitor, has been shown to lower the risk of prostate cancer, though it seems to mostly prevent low-grade tumors. The effect of COX-2 inhibitors such as rofecoxib and celecoxib upon the risk of colon polyps have been studied in familial adenomatous polyposis patients and in the general population. In both groups, there were significant reductions in colon polyp incidence, but this came at the price of increased cardiovascular toxicity.
Genetic testing
Genetic testing for high-risk individuals is already available for certain cancer-related genetic mutations. Carriers of genetic mutations that increase risk for cancer incidence can undergo enhanced surveillance, chemoprevention, or risk-reducing surgery. Early identification of inherited genetic risk for cancer, along with cancer-preventing interventions such as surgery or enhanced surveillance, can be lifesaving for high-risk individuals.
| Gene | Cancer types | Availability |
| BRCA1, BRCA2 | Breast, ovarian, pancreatic | Commercially available for clinical specimens |
| MLH1, MSH2, MSH6, PMS1, PMS2 | Colon, uterine, small bowel, stomach, urinary tract | Commercially available for clinical specimens |
Vaccination
Prophylactic vaccines have been developed to prevent infection by oncogenic infectious agents such as viruses, and therapeutic vaccines are in development to stimulate an immune response against cancer-specific epitopes.
As reported above, a preventive human papillomavirus vaccine exists that targets certain sexually transmitted strains of human papillomavirus that are associated with the development of cervical cancer and genital warts. The only two HPV vaccines on the market as of October 2007 are Gardasil and Cervarix. There is also a hepatitis B vaccine, which prevents infection with the hepatitis B virus, an infectious agent that can cause liver cancer. A canine melanoma vaccine has also been developed.
Screening
Cancer screening is an attempt to detect unsuspected cancers in an asymptomatic population. Screening tests suitable for large numbers of healthy people must be relatively affordable, safe, noninvasive procedures with acceptably low rates of false positive results. If signs of cancer are detected, more definitive and invasive follow up tests are performed to confirm the diagnosis.
Screening for cancer can lead to earlier diagnosis in specific cases. Early diagnosis may lead to extended life, but may also falsely prolong the lead time to death through lead time bias or length time bias.
A number of different screening tests have been developed for different malignancies. Breast cancer screening can be done by breast self-examination, though this approach was discredited by a 2005 study in over 300,000 Chinese women. Screening for breast cancer with mammograms has been shown to reduce the average stage of diagnosis of breast cancer in a population. Stage of diagnosis in a country has been shown to decrease within ten years of introduction of mammographic screening programs. Colorectal cancer can be detected through fecal occult blood testing and colonoscopy, which reduces both colon cancer incidence and mortality, presumably through the detection and removal of pre-malignant polyps. Similarly, cervical cytology testing (using the Pap smear) leads to the identification and excision of precancerous lesions. Over time, such testing has been followed by a dramatic reduction of cervical cancer incidence and mortality. Testicular self-examination is recommended for men beginning at the age of 15 years to detect testicular cancer. Prostate cancer can be screened using a digital rectal exam along with prostate specific antigen (PSA) blood testing, though some authorities (such as the US Preventive Services Task Force) recommend against routinely screening all men.
Screening for cancer is controversial in cases when it is not yet known if the test actually saves lives. The controversy arises when it is not clear if the benefits of screening outweigh the risks of follow-up diagnostic tests and cancer treatments. For example: when screening for prostate cancer, the PSA test may detect small cancers that would never become life threatening, but once detected will lead to treatment. This situation, called overdiagnosis, puts men at risk for complications from unnecessary treatment such as surgery or radiation. Follow up procedures used to diagnose prostate cancer (prostate biopsy) may cause side effects, including bleeding and infection. Prostate cancer treatment may cause incontinence (inability to control urine flow) and erectile dysfunction (erections inadequate for intercourse). Similarly, for breast cancer, there have recently been criticisms that breast screening programs in some countries cause more problems than they solve. This is because screening of women in the general population will result in a large number of women with false positive results which require extensive follow-up investigations to exclude cancer, leading to having a high number-to-treat (or number-to-screen) to prevent or catch a single case of breast cancer early.
Cervical cancer screening via the Pap smear has the best cost-benefit profile of all the forms of cancer screening from a public health perspective as, largely caused by a virus, it has clear risk factors (sexual contact), and the natural progression of cervical cancer is that it normally spreads slowly over a number of years therefore giving more time for the screening program to catch it early. Moreover, the test is easy to perform and relatively cheap.
For these reasons, it is important that the benefits and risks of diagnostic procedures and treatment be taken into account when considering whether to undertake cancer screening.
Use of medical imaging to search for cancer in people without clear symptoms is similarly marred with problems. There is a significant risk of detection of what has been recently called an incidentaloma – a benign lesion that may be interpreted as a malignancy and be subjected to potentially dangerous investigations. Recent studies of CT scan-based screening for lung cancer in smokers have had equivocal results, and systematic screening is not recommended as of July 2007. Randomized clinical trials of plain-film chest X-rays to screen for lung cancer in smokers have shown no benefit for this approach.
Canine cancer detection has shown promise, but is still in the early stages of research.