Breast cancer (malignant breast neoplasm) is cancers originating from breast tissue, most commonly from the inner lining of milk ducts or the lobules that supply the ducts with milk. Cancers originating from ducts are known as ductal carcinomas; those originating from lobules are known as lobular carcinomas. There are many different types of breast cancer, with different stages (spread), aggressiveness, and genetic makeup; survival varies greatly depending on those factors. Computerized models are available to predict survival. With best treatment and dependent on staging, 10-year disease-free survival varies from 98% to 10%. Treatment includes surgery, drugs (hormonal therapy and chemotherapy), and radiation.
Worldwide, breast cancer comprises 10.4% of all cancer incidence among women, making it the most common type of non-skin cancer in women and the fifth most common cause of cancer death. In 2004, breast cancer caused 519,000 deaths worldwide (7% of cancer deaths; almost 1% of all deaths). Breast cancer is about 100 times more common in women than in men, although males tend to have poorer outcomes due to delays in diagnosis.
Some breast cancers require the hormones estrogen and progesterone to grow, and have receptors for those hormones. After surgery those cancers are treated with drugs that interfere with those hormones, usually tamoxifen, and with drugs that shut off the production of estrogen in the ovaries or elsewhere; this may damage the ovaries and end fertility. After surgery, low-risk, hormone-sensitive breast cancers may be treated with hormone therapy and radiation alone. Breast cancers without hormone receptors, or which have spread to the lymph nodes in the armpits, or which express certain genetic characteristics, are higher-risk, and are treated more aggressively. One standard regimen, popular in the U.S., is cyclophosphamide plus doxorubicin (Adriamycin), known as CA; these drugs damage DNA in the cancer, but also in fast-growing normal cells where they cause serious side effects. Sometimes a taxane drug, such as docetaxel, is added, and the regime is then known as CAT; taxane attacks the microtubules in cancer cells. An equivalent treatment, popular in Europe, is cyclophosphamide, methotrexate, and fluorouracil (CMF). Monoclonal antibodies, such as trastuzumab (Herceptin), are used for cancer cells that have the HER2 mutation. Radiation is usually added to the surgical bed to control cancer cells that were missed by the surgery, which usually extends survival, although radiation exposure to the heart may cause damage and heart failure in the following years.
What are the Causes for Breast Cancer?
Research is ongoing to identify the exact causes of breast cancer. Researchers have, however, identified several breast cancer risk factors. A risk factor is something that increases the chance that a person will develop a disease. It is not a guarantee and does not predict a future diagnosis. Risk factors for breast cancer include:
Age: As we grow older, our risk of developing breast cancer increases. It is estimated that 80% of women diagnosed with breast cancer are 50 or older. This doesn’t mean that younger women aren’t at risk. Young women are diagnosed with breast cancer, just much less frequently.
Family and Personal History of Breast Cancer. Having a mother, sister, or daughter with breast cancer doubles your risk of the disease. While family history can play a role in breast cancer development, women shouldn’t subscribe to the popular belief that women without a family history of breast cancer aren’t at risk. The American Cancer Society estimates that 70 to 80% of women with breast cancer do not have a family history that includes breast cancer.
Women who have previously been diagnosed and treated for breast cancer are at a greater risk of developing breast cancer again.
Race. Of all women, Caucasian women are diagnosed more frequently than women of other races. Though Caucasian women are the most at risk, it is African American women who die of the disease the most. Asian, Native American, and Hispanic women have less of a risk.
Alcohol Consumption. Women who drink alcohol increase their breast cancer risk and the risk is heightened with the amount of alcohol consumed. Women who drink 2-5 drinks a day increase their risk by 1 1/2 when compared to women who do not drink alcohol. One drink a day only slightly elevates a woman’s risk.
Family Planning Choices. Women who choose not to have children or have them after age 30 somewhat increase their risk of breast cancer.
Genetics Genetics may play a role in up to 10% of women diagnosed with breast cancer. Hereditary breast cancer occurs when a mutated gene has been passed down from a parent. The most common genetic mutation is that of the BRCA gene pair, referred to as “BRCA1″ and “BRCA2″. These genes are responsible for regulating cell growth and repairing damaged DNA, but do not properly function if mutated. Those who are found through genetic testing to be carriers of mutated BRCA genes are at an increased risk of developing breast cancer. Other gene types have been associated to breast cancer, but not as prevalently as the BRCA genes.
There are several other breast cancer risk factors, such as use of hormone replacement therapy, obesity, and oral contraceptive use.
What are the Symptoms of Breast Cancer?
The first noticeable symptom of breast cancer is typically a lump that feels different from the rest of the breast tissue. More than 80% of breast cancer cases are discovered when the woman feels a lump. By the time a breast lump is noticeable, it has probably been growing for years. The earliest breast cancers are detected by a mammogram. Lumps found in lymph nodes located in the armpits can also indicate breast cancer.
Indications of breast cancer other than a lump may include changes in breast size or shape, skin dimpling, nipple inversion, or spontaneous single-nipple discharge. Pain (“mastodynia”) is an unreliable tool in determining the presence or absence of breast cancer, but may be indicative of other breast health issues.
When breast cancer cells invade the dermal lymphatics—small lymph vessels in the skin of the breast—its presentation can resemble skin inflammation and thus is known as inflammatory breast cancer (IBC). Symptoms of inflammatory breast cancer include pain, swelling, warmth and redness throughout the breast, as well as an orange-peel texture to the skin referred to as peau d’orange.
Another reported symptom complex of breast cancer is Paget’s disease of the breast. This syndrome presents as eczematoid skin changes such as redness and mild flaking of the nipple skin. As Paget’s advances, symptoms may include tingling, itching, increased sensitivity, burning, and pain. There may also be discharge from the nipple. Approximately half of women diagnosed with Paget’s also have a lump in the breast.
Occasionally, breast cancer presents as metastatic disease, that is, cancer that has spread beyond the original organ. Metastatic breast cancer will cause symptoms that depend on the location of metastasis. Common sites of metastasis include bone, liver, lung and brain. Unexplained weight loss can occasionally herald an occult breast cancer, as can symptoms of fevers or chills. Bone or joint pains can sometimes be manifestations of metastatic breast cancer, as can jaundice or neurological symptoms. These symptoms are “non-specific”, meaning they can also be manifestations of many other illnesses.
Most symptoms of breast disorder do not turn out to represent underlying breast cancer. Benign breast diseases such as mastitis and fibroadenoma of the breast are more common causes of breast disorder symptoms. The appearance of a new symptom should be taken seriously by both patients and their doctors, because of the possibility of an underlying breast cancer at almost any age.
What are the Risk Factors?
The primary risk factors that have been identified are sex, age, lack of childbearing or breastfeeding, and higher hormone levels.
In Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective, a 2007 report by American Institute for Cancer Research/ World Cancer Research Fund, it concluded women can reduce their risk by maintaining a healthy weight, drinking less alcohol, being physically active and breastfeeding their children. This was based on an review of 873 separate studies.
In 2009 World Cancer Research Fund announced the results of a further review review that took into account a further 81 studies published subsequently. This did not change the conclusions of the 2007 Report. In 2009, WCRF/ AICR published Policy and Action for Cancer Prevention, a Policy Report that included a preventability study. This estimated that 38% of breast cancer cases in the US are preventable through reducing alcohol intake, increasing physical activity levels and maintaining a healthy weight. It also estimated that 42% of breast cancer cases in the UK could be prevented in this way, as well as 28% in Brazil and 20% in China.
In a study published in 1995, well-established risk factors accounted for 47% of cases while only 5% were attributable to hereditary syndromes. Genetic factors usually increase the risk slightly or moderately; the exception is women and men who are carriers of BRCA mutations. These people have a very high lifetime risk for breast and ovarian cancer, depending on the portion of the proteins where the mutation occurs. Instead of a 12 percent lifetime risk of breast cancer, women with one of these genes has a risk of approximately 60 percent. In more recent years, research has indicated the impact of diet and other behaviors on breast cancer. These additional risk factors include a high-fat diet, alcohol intake, obesity, and environmental factors such as tobacco use, radiation, endocrine disruptors and shiftwork. Although the radiation from mammography is a low dose, the cumulative effect can cause cancer.
In addition to the risk factors specified above, demographic and medical risk factors include:
- Personal history of breast cancer: A woman who had breast cancer in one breast has an increased risk of getting cancer in her other breast.
- Family history: A woman’s risk of breast cancer is higher if her mother, sister, or daughter had breast cancer. The risk is higher if her family member got breast cancer before age 40. Having other relatives with breast cancer (in either her mother’s or father’s family) may also increase a woman’s risk.
- Certain breast changes: Some women have cells in the breast that look abnormal under a microscope. Having certain types of abnormal cells (atypical hyperplasia and lobular carcinoma in situ [LCIS]) increases the risk of breast cancer.
- Race: Breast cancer is diagnosed more often in women of European ancestry than those of African or Asian ancestry.
A National Cancer Institute (NCI) study of 72,000 women found that those who had a normal body mass index at age 20 and gained weight as they aged had nearly double the risk of developing breast cancer after menopause in comparison to women maintained their weight. The average 60 year-old woman’s risk of developing breast cancer by age 65 is about 2 percent; her lifetime risk is 13 percent.
Abortion has not been found to be a risk factor for breast cancer. The breast cancer abortion hypothesis, however, continues to be promoted by some pro-life groups.
The United Kingdom is the member of International Cancer Genome Consortium that is leading efforts to map breast cancer’s complete genome.
Classification
Breast cancers can be classified by different schemata. Every aspect influences treatment response and prognosis. Description of a breast cancer would optimally include multiple classification aspects, as well as other findings, such as signs found on physical exam. Classification aspects include stage (TNM), pathology, grade, receptor status, and the presence or absence of genes as determined by DNA testing:
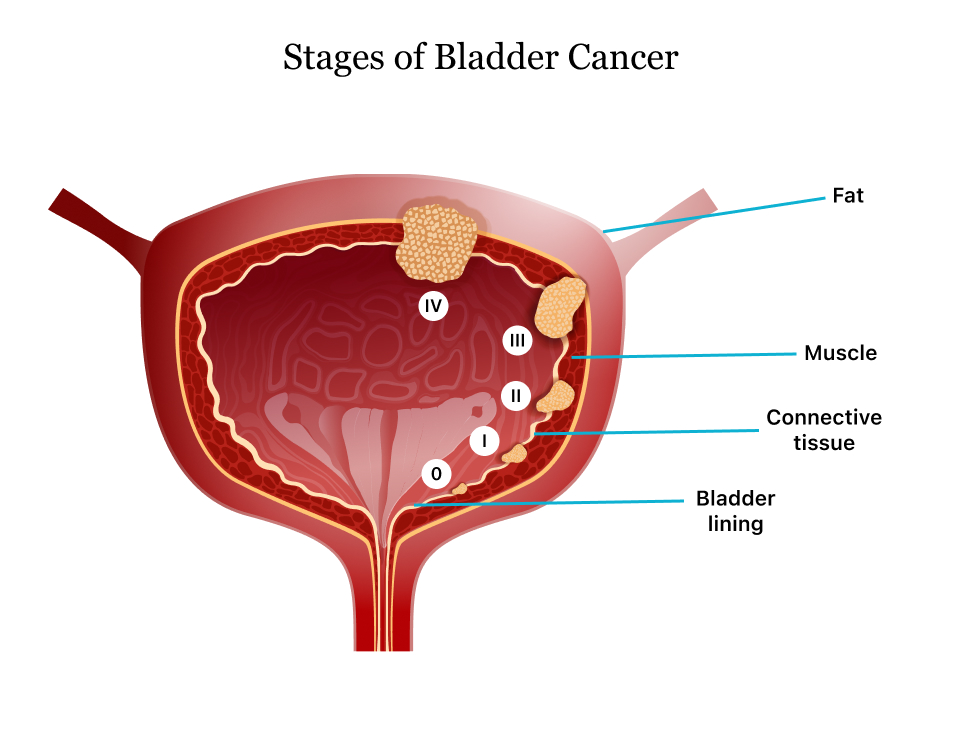
- Stage. The TNM classification for breast cancer is based on the size of the tumor (T), whether or not the tumor has spread to the lymph nodes (N) in the armpits, and whether the tumor has metastasized (M) (i.e. spread to a more distant part of the body). Larger size, nodal spread, and metastasis have a larger stage number and a worse prognosis.
The main stages are:
Stage 0 is a pre-malignant disease or marker (sometimes called DCIS: Ductal Carcinoma in Situ) .
Stages 1–3 are defined as ‘early’ cancer and potentially curable.
Stage 4 is defined as ‘advanced’ and/or ‘metastatic’ cancer and incurable.
- Histopathology. Breast cancer is usually, but not always, primarily classified by its histological appearance. Most breast cancers are’ derived from the epithelium lining the ducts or lobules, and are classified as mammary ductal carcinoma. Carcinoma in situ is proliferation of cancer cells within the epithelial tissue without invasion of the surrounding tissue. In contrast, invasive carcinoma invades the surrounding tissue.
- Grade (Bloom-Richardson grade). When cells become differentiated, they take different shapes and forms to function as part of an organ. Cancerous cells lose that differentiation. In cancer grading, tumor cells are generally classified as well differentiated (low grade), moderately differentiated (intermediate grade), and poorly differentiated (high grade). Poorly differentiated cancers have a worse prognosis.
- Receptor status. Cells have receptors on their surface and in their cytoplasm and nucleus. Chemical messengers such as hormones bind to receptors, and this causes changes in the cell. Breast cancer cells may or may not have three important receptors: estrogen receptor (ER), progesterone receptor (PR), and HER2/neu. Cells with none of these receptors are called basal-like or triple negative. ER+ cancer cells depend on estrogen for their growth, so they can be treated with drugs to block estrogen effects (e.g. tamoxifen), and generally have a better prognosis.
Generally, HER2+ had a worse prognosis, however HER2+ cancer cells respond to drugs such as the monoclonal antibody, trastuzumab, (in combination with conventional chemotherapy) and this has improved the prognosis significantly.
- DNA microarrays have compared normal cells to breast cancer cells and found differences in hundreds of genes, but the significance of most of those differences is unknown.
Diagnosis of Breast Cancer
While screening techniques (which are further discussed below) are useful in determining the possibility of cancer, a further testing is necessary to confirm whether a lump detected on screening is cancer, as opposed to a benign alternative such as a simple cyst.
In a clinical setting, breast cancer is commonly diagnosed using a “triple test” of clinical breast examination (breast examination by a trained medical practitioner), mammography, and fine needle aspiration cytology. Both mammography and clinical breast exam, also used for screening, can indicate an approximate likelihood that a lump is cancer, and may also identify any other lesions. Fine Needle Aspiration and Cytology (FNAC), which may be done in a GP’s office using local anaesthetic if required, involves attempting to extract a small portion of fluid from the lump. Clear fluid makes the lump highly unlikely to be cancerous, but bloody fluid may be sent off for inspection under a microscope for cancerous cells. Together, these three tools can be used to diagnose breast cancer with a good degree of accuracy.
Other options for biopsy include core biopsy, where a section of the breast lump is removed, and an excisional biopsy, where the entire lump is removed.
In addition vacuum-assisted breast biopsy (VAB) may help diagnose breast cancer among patients with a mammographically detected breast in women according to a systematic review. In this study, summary estimates for vacuum assisted breast biopsy in diagnosis of breast cancer were as follows sensitivity was 98.1% with 95% CI = 0.972-0.987 and specificity was 100% with 95% CI = 0.997-0.999. However underestimate rates of atypical ductal hyperplasia (ADH) and ductal carcinoma in situ (DCIS) were 20.9% with 95% CI =0.177-0.245 and 11.2% with 95% CI = 0.098-0.128 respectively.
Screening
Breast cancer screening refers to testing otherwise-healthy women for breast cancer in an attempt to achieve an earlier diagnosis. The assumption is that early detection will improve outcomes. A number of screening test have been employed including: clinical and self breast exams, mammography, genetic screening, ultrasound, and magnetic resonance imaging.
A clinical or self breast exam involves feeling the breast for lumps or other abnormalities. Research evidence does not support the effectiveness of either type of breast exam, because by the time a lump is large enough to be found it is likely to have been growing for several years and will soon be large enough to be found without an exam. Mammographic screening for breast cancer uses x-rays to examine the breast for any uncharacteristic masses or lumps. The Cochrane collaboration in 2009 concluded that mammograms reduce mortality from breast cancer by 15 percent but also result in unnecessary surgery and anxiety, resulting in their view that mammography screening may do more harm than good. Many national organizations recommend regular mammography, nevertheless. For the average woman, the U.S. Preventive Services Task Force recommends mammography every two years in women between the ages of 50 and 74. The Task Force points out that in addition to unnecessary surgery and anxiety, the risks of more frequent mammograms include a small but significant increase in breast cancer induced by radiation.
In women at high risk, such as those with a strong family history of cancer, mammography screening is recommended at an earlier age and additional testing may include genetic screening that tests for the BRCA genes and / or magnetic resonance imaging.
Methods of Treatment for Breast Cancer
Surgery. Most women with breast cancer will have surgery to remove cancerous tissue and for diagnostic purposes. Types of surgery used to treat breast cancer include:
- lumpectomy
- quadrantectomy
- mastectomy
Chemotherapy. The organs in our body are made up of cells. Cells divide and multiply as the body needs them. When these cells continue multiplying when the body doesn’t need them, the result is a mass or growth, also called a tumor. Chemotherapy drugs work by eliminating these rapidly multiplying renegade cells. There are other healthy cells in the body that multiply just as quickly, like hair follicle cells. Unfortunately, many chemotherapy drugs may not be able to discern the two, attacking healthy cells and causing side effects like hair loss.
In breast cancer, chemotherapy is used to treat the cancer and also to prevent it from returning once it has been treated. Women who have been diagnosed with stages II through IV breast cancer are most commonly given chemotherapy, however some women diagnosed with stage I breast cancer may benefit from chemotherapy treatment.
Radiation Therapy. Radiation therapy uses certain types high energy beams of radiation to shrink tumors or eliminate cancer cells. Radiation therapy works by damaging a cancer cell’s DNA, making it unable to multiply. Although radiation therapy can damage nearby healthy cells, cancer cells are highly sensitive to radiation and typically die when treated. Healthy cells that are damaged during radiation are resilient and are often able to fully recover.
There are two primary types of radiation therapy: external beam radiation therapy and internal beam radiation, also called brachytherapy. In breast cancer, external beam radiation is much more common than internal beam radiation.
Targeted Therapy. This type of therapy is less harmful to healthy cells than chemotherapy and targets properties of cancer cells that allow for rapid uncontrolled cell growth. This type of therapy is given in tablet form or in a chemotherapy infusion. Targeted therapy often accompanies chemotherapy in the breast cancer treatment plan. Drugs used for targeted therapy include:
- Herceptin
- Tykerb
- Avastin
Hormonal Therapy. In many cases of breast cancer, the cancer growth is fueled by the hormone estrogen that is produced by the ovaries. Hormonal therapy, also referred as anti-estrogen therapy, deprives estrogen of its ability to stimulate growth in breast cancer cells. Hormonal therapy is given to treat breast cancer and prevent recurrence.
The ovaries are the primary site of estrogen production, so hormonal treatment can include an oopherectomy, the surgical removal of the ovaries. Halting the ovary’s production of estrogen through drugs may also be an option. Removal of the the ovaries and therapy to block estrogen production are recommended for pre-menopausal women with estrogen-receptor positive breast cancer or for women who have advanced breast cancer.
Aromatase inhibitors are another form of hormonal therapy used in post-menopausal women who have had estrogen-receptor positive breast cancer. It is given as a follow-up therapy to prevent recurrence.
Women’s bodies produce an enzyme called aromatase that allows androgens to convert to a type of estrogen. Aromatase inhibitors suppress the this enzyme, lowering the levels of estrogen in the body. Types of aromatase inhibitor drugs include:
- Arimidex
- Aromasin
- Femara
Selective estrogen receptor modulators (SERM) are another form of hormonal treatment used in women with estrogen receptor positive breast cancer. SERMs work by preventing natural estrogen from sending signals to the estrogen receptor. In simplified terms, SERMs rush to the estrogen receptor and take the place where natural estrogen would like to occupy. Some like to compare it to musical chairs or two jigsaw puzzle pieces. There are three SERMs that are currently prescribed:
- Evista
- Fareston
- Tamoxifen
Drugs rating:
| Title | Votes | Rating | ||
| 1 | Cenestin (Conjugated Estrogens) | 8 |
|
(10.0/10) |
| 2 | Menest (Esterified Estrogens) | 1 |
|
(10.0/10) |
| 3 | Adriamycin (Doxorubicin) | 11 |
|
(8.9/10) |
| 4 | Estrace (Estradiol) | 16 |
|
(8.3/10) |
| 5 | Megace (Megestrol) | 3 |
|
(8.3/10) |
| 6 | Enjuvia (Conjugated Estrogens) | 20 |
|
(8.2/10) |
| 7 | Xeloda (Capecitabine) | 25 |
|
(8.1/10) |
| 8 | Premarin (Conjugated Estrogens) | 57 |
|
(8.0/10) |
| 9 | Nolvadex (Tamoxifen) | 3 |
|
(8.0/10) |
| 10 | Arimidex (Anastrozole) | 145 |
|
(7.8/10) |
| 11 | Herceptin (Trastuzumab) | 36 |
|
(7.7/10) |
| 12 | Faslodex (Fulvestrant) | 25 |
|
(7.7/10) |
| 13 | Soltamox (Tamoxifen) | 2 |
|
(7.5/10) |
| 14 | Aromasin (Exemestane) | 78 |
|
(7.2/10) |
| 15 | Cytoxan (Cyclophosphamide) | 42 |
|
(7.0/10) |
| 16 | Avastin (Bevacizumab) | 13 |
|
(6.8/10) |
| 17 | Femara (Letrozole) | 75 |
|
(6.7/10) |
| 18 | Methotrexate | 231 |
|
(6.5/10) |
| 19 | Zoladex (Goserelin) | 47 |
|
(6.2/10) |
| 20 | Taxol (Paclitaxel) | 13 |
|
(6.0/10) |
| 21 | Tamoxifen | 2 |
|
(6.0/10) |
| 22 | Taxotere (Docetaxel) | 6 |
|
(4.3/10) |
| 23 | Ixempra (Ixabepilone) | 0 |
|
(0/10) |
| 24 | Fareston (Toremifene) | 0 |
|
(0/10) |
| 25 | Androxy (Fluoxymesterone) | 0 |
|
(0/10) |
| 26 | Gemzar (Gemcitabine) | 0 |
|
(0/10) |
| 27 | Abraxane (Paclitaxel) | 0 |
|
(0/10) |
| 28 | Megace Suspension (Megestrol) | 0 |
|
(0/10) |
| 29 | Gynodiol (Estradiol) | 0 |
|
(0/10) |
| 30 | Estratab (Esterified Estrogens) | 0 |
|
(0/10) |
| 31 | Adrucil (Fluorouracil) | 0 |
|
(0/10) |
| 32 | Cytadren (Aminoglutethimide) | 0 |
|
(0/10) |
| 33 | Thioplex (Thiotepa) | 0 |
|
(0/10) |
| 34 | Thiotepa | 0 |
|
(0/10) |
| 35 | Trexall (Methotrexate) | 0 |
|
(0/10) |
| 36 | Velban (Vinblastine) | 0 |
|
(0/10) |
| 37 | Vinblastine | 0 |
|
(0/10) |
| 38 | Tykerb (Lapatinib) | 0 |
|
(0/10) |
| 39 | Neosar (Cyclophosphamide) | 0 |
|
(0/10) |
| 40 | Onxol (Paclitaxel) | 0 |
|
(0/10) |
Prognosis
A prognosis is a prediction of outcome and the probability of progression-free survival (PFS) or disease-free survival (DFS). These predictions are based on experience with breast cancer patients with similar classification. A prognosis is an estimate, as patients with the same classification will survive a different amount of time, and classifications are not always precise. Survival is usually calculated as an average number of months (or years) that 50% of patients survive, or the percentage of patients that are alive after 1, 5, 15 and 20 years. Prognosis is important for treatment decisions because patients with a good prognosis are usually offered less invasive treatments, such as lumpectomy and radiation or hormone therapy, while patients with poor prognosis are usually offered more aggressive treatment, such as more extensive mastectomy and one or more chemotherapy drugs.
Prognostic factors include staging, (i.e., tumor size, location, grade, whether disease has traveled to other parts of the body), recurrence of the disease, and age of patient.
Stage is the most important, as it takes into consideration size, local involvement, lymph node status and whether metastatic disease is present. The higher the stage at diagnosis, the worse the prognosis. The stage is raised by the invasiveness of disease to lymph nodes, chest wall, skin or beyond, and the aggressiveness of the cancer cells. The stage is lowered by the presence of cancer-free zones and close-to-normal cell behaviour (grading). Size is not a factor in staging unless the cancer is invasive. For example, Ductal Carcinoma In Situ (DCIS) involving the entire breast will still be stage zero and consequently an excellent prognosis with a 10yr disease free survival of about 98%.
Grading is based on how biopsied, cultured cells behave. The closer to normal cancer cells are, the slower their growth and the better the prognosis. If cells are not well differentiated, they will appear immature, will divide more rapidly, and will tend to spread. Well differentiated is given a grade of 1, moderate is grade 2, while poor or undifferentiated is given a higher grade of 3 or 4 (depending upon the scale used).
Younger women tend to have a poorer prognosis than post-menopausal women due to several factors. Their breasts are active with their cycles, they may be nursing infants, and may be unaware of changes in their breasts. Therefore, younger women are usually at a more advanced stage when diagnosed. There may also be biologic factors contributing to a higher risk of disease recurrence for younger women with breast cancer.
The presence of estrogen and progesterone receptors in the cancer cell is important in guiding treatment. Those who do not test positive for these specific receptors will not be able to respond to hormone therapy, and this can affect their chance of survival depending upon what treatment options remain, the exact type of the cancer, and how advanced the disease is.
In addition to hormone receptors, there are other cell surface proteins that may affect prognosis and treatment. HER2 status directs the course of treatment. Patients whose cancer cells are positive for HER2 have more aggressive disease and may be treated with the ‘targeted therapy’, trastuzumab (Herceptin), a monoclonal antibody that targets this protein and improves the prognosis significantly. Tumors overexpressing the Wnt signaling pathway co-receptor low-density lipoprotein receptor-related protein 6 (LRP6) may represent a distinct subtype of breast cancer and a potential treatment target.
Psychological aspects
The emotional impact of cancer diagnosis, symptoms, treatment, and related issues can be severe. Most larger hospitals are associated with cancer support groups which provide a supportive environment to help patients cope and gain perspective from cancer survivors. Online cancer support groups are also very beneficial to cancer patients, especially in dealing with uncertainty and body-image problems inherent in cancer treatment.
Not all breast cancer patients experience their illness in the same manner. Factors such as age can have a significant impact on the way a patient copes with a breast cancer diagnosis. Premenopausal women with estrogen-receptor positive breast cancer must confront the issues of early menopause induced by many of the chemotherapy regimens used to treat their breast cancer, especially those that use hormones to counteract ovarian function.
On the other hand, a recent study conducted by researchers at the College of Public Health of the University of Georgia showed that older women may face a more difficult recovery from breast cancer than their younger counterparts. As the incidence of breast cancer in women over 50 rises and survival rates increase, breast cancer is increasingly becoming a geriatric issue that warrants both further research and the expansion of specialized cancer support services tailored for specific age groups.
Breast Cancer Prevention
Unfortunately, there are no true methods of preventing breast cancer, but by avoiding breast cancer risk factors, you can decrease your risk of developing it. Because simply being a woman is a risk for developing breast cancer, women must be proactive in taking care of their breasts by:
- doing self breast exams at home, beginning in their 20s
- having yearly clinical breast exam by a nurse or doctor in their 20s and 30s
- having a annual mammogram, beginning at age 40 (women at a higher risk may begin having mammograms earlier at the recommendation of their doctor)
Women who are classified as being at very high risk for breast cancer may choose more drastic, yet appropriate, means of reducing their risk. Prophylactic oophorectomy (removal of the ovaries) and/or prophylactic mastectomy may be a prevention method for women in this risk category. Although these methods can certainly reduce a woman’s risk of developing breast cancer, it is by no means a guarantee.